A lived-experience focus group quoted in the report said the use of compulsory community treatment orders was fundamentally disempowering process. Photo: Marika Khabazi
The Mental Health and Wellbeing Commission is calling for the use of compulsory community treatment orders to be reduced.
Analysing the lived experience of those who had faced a compulsory order, a report from the commission, Te Hiringa Mahara, said the law was outdated and not aligned with international human rights obligations.
Compulsory community treatment orders (CCTOs) can be granted by a judge under the Mental Health Act, compelling a patient to attend or take treatment (typically medication), at the direction of a clinician.
The person must accept the treatment for up to six months, but this can be extended.
Te Hiringa Mahara board chair Hayden Wano said over the past five years, judges granted nearly 90 percent of applications made by clinicians.
The report said the number of people subjected to a CCTO had increased by eight percent between 2017 and 2021, meaning in 2021 almost 7000 people were under compulsory treatment.
"They can be people who are going to work, it can be students who are going to university, there could be a number of people who are going about their normal life who are required to have enforced treatment as a result of this order," Wano said.
A lived-experience focus group quoted in the report said it was a fundamentally disempowering process.
"So often it seems to be that the decision's already been made... the judge's doctor has already formed the opinion."
People told Te Hiringa Mahara they found the process traumatising, and it made them feel like a criminal, particularly when they had to go before a judge.

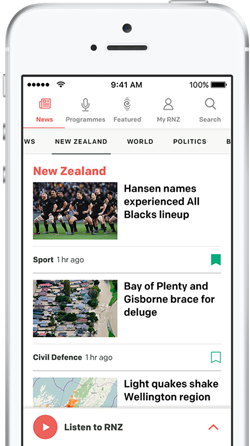
Te Hiringa Mahara board chair Hayden Wano. Photo: supplied
Wano said Māori were subject to the orders more than any other group.
The report said tāngata whai ora (people who are the subject of care or treatment), whānau, and family were excluded from participation in the processes.
"The weight of opinion goes towards the clinician. And as some whānau have said, their voices are silenced in both the clinical process as well as in the court process," Wano said.
"So what we're advocating for is a supportive decision-making process whereby people in the system, whether they be whānau, their GP, their community-based provider, are also involved, that their voices can be brought into the process to help support this person through the process of getting access to care that they want, that they have a say in."
In 2019, the government accepted the Report of the Government Inquiry into Mental Health and Addiction's recommendation to repeal the Mental Health Act, and replace it with a law better reflecting Crown obligations under Te Tiriti o Waitangi, and New Zealand's international commitments under the United Nations Convention on the Rights of Persons with Disabilities.
While that full process is likely to take a long time, Wano said some changes should occur now, including a reduction in the number of compulsory treatment applications made and granted, a reduction in their use for Māori and Pacific peoples, and for services and courts to hear perspectives of tāngata whai ora, whānau, and family.